Anywhere, anytime: someone may get ill or get seriously injured, thus requiring a medical implant. According to a jointly report published by the American Joint Replacement Registry (AJRR) and the American Academy of Orthopedic Surgeons (AAOS), when one looks at hip and knee replacement procedures, for instance, over 1.7 million hip and knee replacement procedures are performed worldwide on 1.2 million patients per year. Here is the thing, many don’t realize that such implants may eventually fail in 5% to 10% of patients. While no one can be 100% sure that a hip or knee replacement will be the last operation needed on a specific joint, the ultimate goal for medical device manufacturers and healthcare professionals remains to explore all possible solutions that can increase the chances of a long-term successful surgery. One of these solutions lies in the choice of the right materials.
As you may guess, off-the-shelf implants have made it easier for medical professionals to treat the most common patient needs quickly. As technology advances, one realizes that Additive Manufacturing is not just an alternative method for manufacturing hip cups and spine cages at scale; the technology helps to reshape what implants can do, and how patients can be treated. The problem is, very often the use of AM in medical applications is highlighted through the use of metals. Yet, they are not necessarily the ideal materials for every application.
The article below ambitions to highlight the role of polymer AM materials in creating and improving the next generation of 3D printed implants. To do so, we will discuss:
- The use of polymer materials in AM vs the use of polymer materials in conventional manufacturing
- The metals vs polymers choice
Before we dive into this topic, it’s crucial to make the difference between biopolymers and biomaterials.
“Per definition, all materials used for long-term implant applications are biomaterials since they are in contact with body tissue, liquids and/or bone. One crucial requirement for biomaterials should be their excellent biocompatibility.
“Biopolymers” on the other hand are defined as a polymer of biological origin, e.g. microbial. It is not a general requirement for a polymer biomaterial to be a biopolymer”, Marc Knebel, Head of Medical Systems at Evonik lays emphasis on this.
This means that biopolymers can be biocompatible and biodegradable, and can be used in applications that go beyond the healthcare industry; applications such as edible films, emulsions, and packaging materials in the food industry for example.
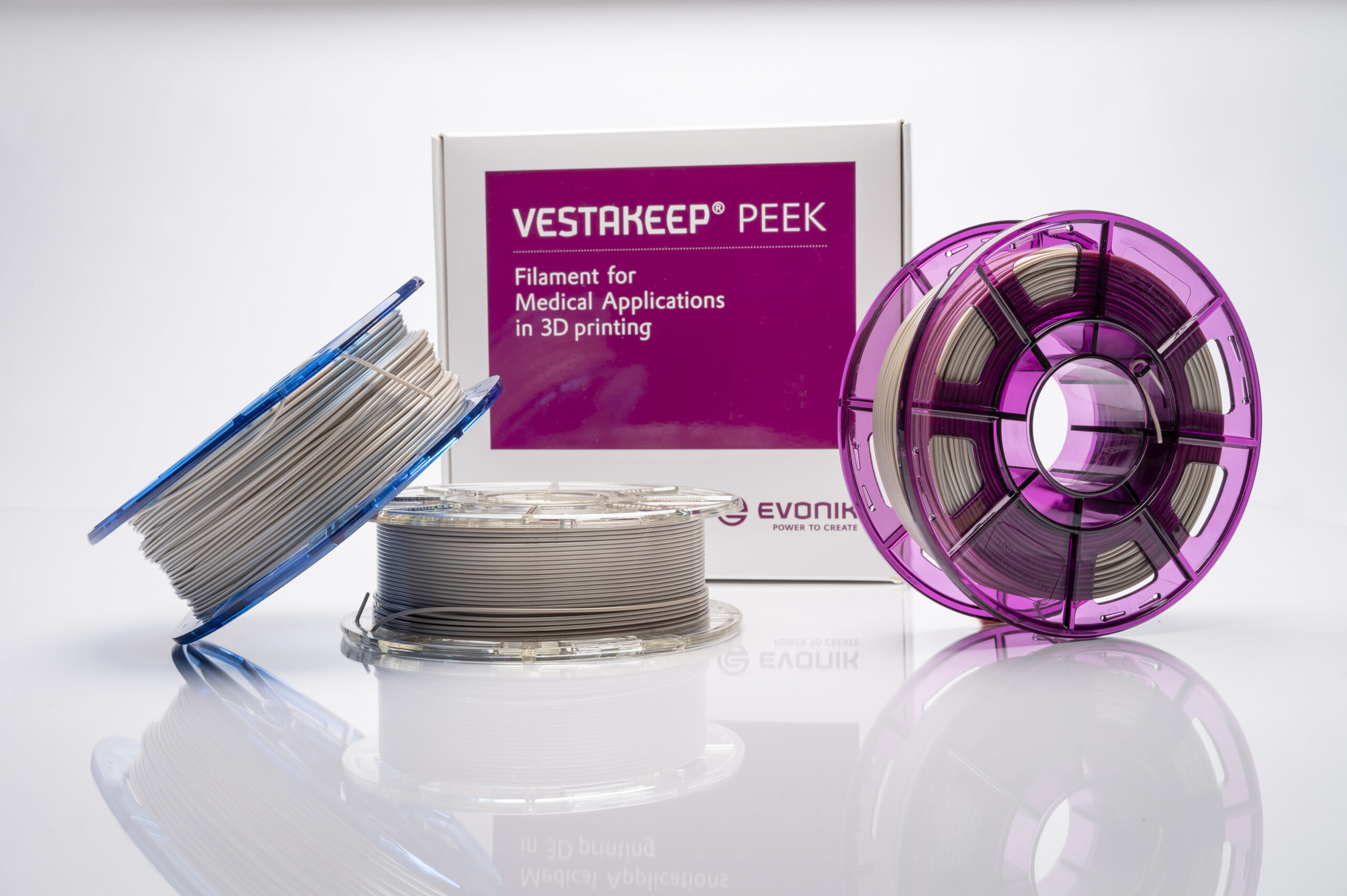
Specialty chemicals company Evonik specifically provides biomaterials of biological as well as non-biological origins. The RESOMER® material is a degradable biopolymer and VESTAKEEP® is a biostable polymer. Both materials can be processed by 3D printing, RESOMER® via SLS, FFF and Freeform printing and VESTAKEEP® via FFF or Freeform printing.
The use of polymer materials in AM vs the use of polymer materials in conventional manufacturing
From a manufacturing standpoint, traditional subtractive manufacturing makes sense for manufacturers who want to produce ready-made solutions that can treat the most common patient needs. However, given the complexity of anatomical structures, such technology rapidly becomes limited in the geometries it can produce, as well as the number of pieces of equipment required to make an implant. Not to mention that the time required for machining can be significant, especially when working with harder metals.
First and foremost, “3D printing of polymer-based implants is not restricted to a particular type of implants. All current implants for which polymers are being used are possible. With the new possibilities of additive technologies, potentially even wider range of applications is achievable. One example shows the company BellaSeno [a developer of 3D printed absorbable scaffolds] uses 3D printed resorbable implants in applications that use silicone (breast implants). The most important is that 3D printed implants fulfill the biocompatibility and mechanical requirements for an implant.
More generally – 3D printing has substantial advantages in two main fields: (1) Patient-specific implants that has an n=1, that is unique to the patient and that conventionally would result in a large amount of material loss, e.g. from machining, easier logistics and less working capital. (2) New designs and functionalities, not achievable with conventional technologies. This includes hollow or porous structures of particular surface properties,” Knebel explains.

As far as materials are concerned, it should be noted that whether they are processed via conventional manufacturing processes (such as injection molding or machining) or via AM, they should deliver the same mechanical properties. That being said, whether we talk about extrusion, resin, and powder 3D printing processes, polymer 3D printing can provide versatility for materials selection and support designs with diverse architectures, responses, and layouts. This is something that the Head of Medical Systems outlines:
“The same quality and documentation for the material are required as it is for any long-term body contact (implant) application. Same as for other processing technologies, all processing steps have to be validated and qualified (IQ/OQ/PQ) and it must be assured that a safe medical device is produced.
The difference, e.g. to injection molding, is that 3D printing offers substantially more variables to adjust in the process and all these parameters have to be checked and validated.”
Needless to say that decisions across the material, the ideal 3D printing process, and design strategies are made in a nonlinear way that requires careful consideration and knowledge of their relation to a given application. Choosing a polymer material, therefore, requires considering a wide range of measurable properties that we cannot assess here. However, for the manufacturing of 3D printed implants, Evonik recommends focusing on “Smart Biomaterials”, a type of material that can combine multiple features.
“One example of this is the VESTAKEEP® Fusion Filament for FFF printing. In this product, we have integrated a bioactive additive that combines the excellent biocompatibility and mechanical properties of PEEK with bioactive properties for faster bone healing and therefore a faster patient recovery”, Knebel explains.
Moreover, from a treatment standpoint, a primary concern all healthcare professionals have is the acceptance of the implant by the patient’s body. AM addresses this concern as it allows for the inclusion of porous structures within the implant, a pivotal attribute that enables the biomedical fusion of the implant.
The metals vs polymers choice
Polymers only make up about 10% of the global implants market; a percentage that seems unfair when one knows the arguments that play to the strengths of these materials in applications related to 3D printed implants.
The high stiffness of metal implants for example can lead to mechanical issues such as stress shielding forces that are transferred from the metal implant on the remaining bone. (Understand here that stress shielding is the reduction in bone density (osteopenia) as a result of removal of typical stress from the bone by a metal implant.) When it comes to safety equipment, polymer-printed lattices achieve efficient energy absorption with a rapid fabrication process that bypasses the supply chain limitations of bulk manufacturing.
To these arguments, Knebel adds the natural flexibility of polymer materials such as PEEK which is close to the natural bone –leading to less stress shielding and eventually to implant loosening. He also mentions the fact there are no image artifacts under the x-ray of MRT. This is even more important for new development in robotic surgery that does not allow image artifacts during the surgery for high precision.
“As a metal-free solution, polymers can be the material of choice for allergy patients.
With respect to the 3D printing of metal implants, the SLS technology is well established. The major obstacle here is the powder handling and subsequent powder removal from the final implant. This very work and time-consuming powder handling and removal limit the use of this technology to a low number of centralized facilities.
The FFF-technology for processing of polymers offers the advantage of decentralized point-of-care implant production, e.g. directly in the hospital. Machines are smaller, filament handling is safe and easy, and post-treatment much easier. Implant production can be directly integrated into the fully digital workflow in the hospital for a faster patient treatment,” He continues.
From a healing standpoint, “healing is generally also well understood and positive for metal materials. However, allergies occur more frequently vs. no allergic reaction is reported for PEEK.
Healing of the implant can be further increased by 3D printing with structure and surface design, e.g., the roughness of porous structures. Also, fast healing materials such as VESTAKEEP Fusion for faster bone growth accelerate the patient recovery”.
Conclusion
Due to their high risks for the end-user and their potential failure, implants are classified into the class III of products subject to general controls by the FDA. Using AM comes with a number of variables that mitigate these risks while providing reasonable assurance of safety and effectiveness. Currently, more than 80% of implants would last longer than 25 years. A research reveals that this number could increase with additively manufactured implants. To continue on this path, a couple of success factors include: a continuous collaboration between material producers and 3D printer manufacturers, “a close connection to key opinion leaders (e.g., surgeons) and OEMs to understand unmet needs; trust in the market and reliable producer of safe materials, as well as a material expertise and backward integration to understand polymer well and having the capabilities and know-how to modify polymer design as needed.”.
This content has been created in collaboration with Evonik.