The first in-house, custom, personalized 3D surgical procedure repaired a distal radius malunion, which is caused when a broken forearm heals incorrectly, resulting in misaligned or deformed bones.
An injury to the forearm can lead to functional impairment of the wrist, loss of strength, a reduced range of motion, pain, and cosmetic concerns. Malunions typically occur because of inadequate immobilization, poor fracture reduction, or underlying medical conditions that impact the process of healing bone.
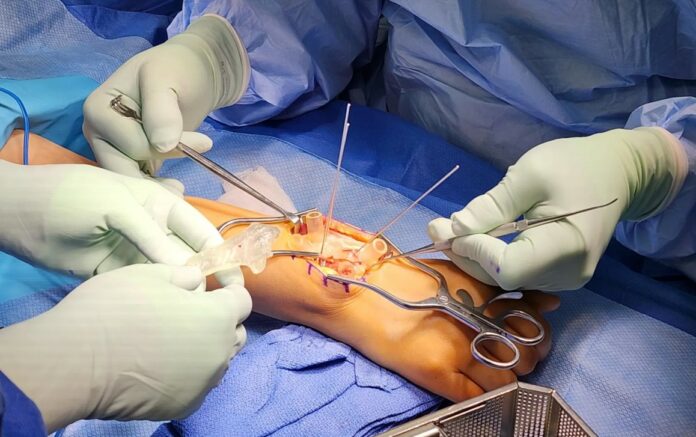
The most common surgical procedure to repair a malunion is called an osteotomy. During the operation, a surgeon will cut the affected bones and move them into a better position and hold them in place with a plate and screws intended to keep the forearm stable while it heals. In the past, these cases were corrected “freehand” using the surgeon’s best judgment and X-rays to reposition the bone. However, realigning in all three planes of the deformity is not possible based on X-rays alone. Now, with the use of 3D planning, the deformity and anatomy can be corrected back to exactly how they were before the injury.
Lisa Lattanza, MD, Chair and Ensign Professor of Orthopaedics & Rehabilitation, performed this surgery at Yale School of Medicine. Its completion made a real splash as this was the first in-house, custom, personalized 3D surgical procedure.
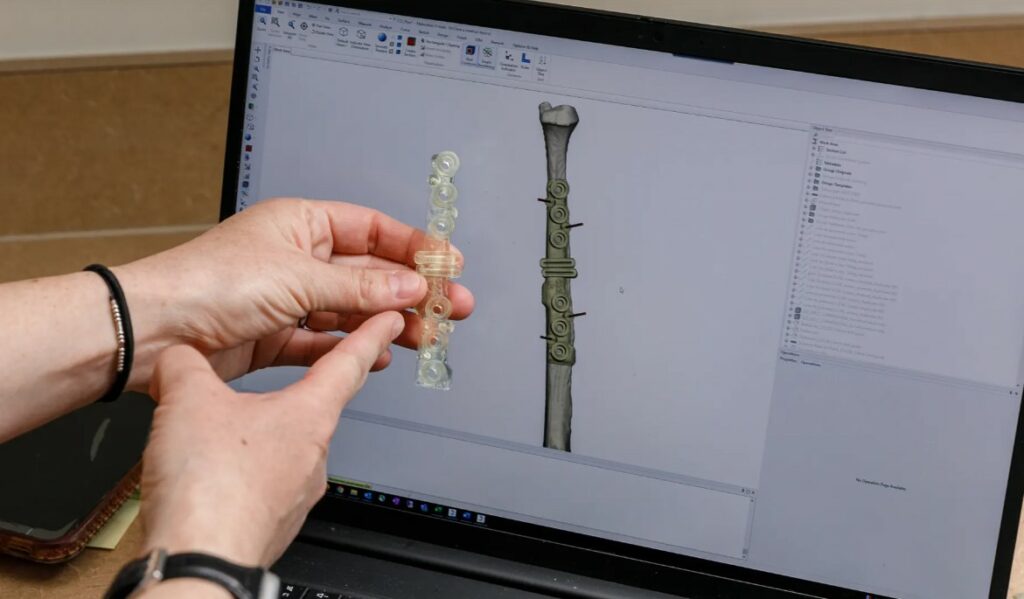
Lattanza worked alongside a Yale team to develop a 3D surgical plan for the patient, 3D printed personalized surgical guides, and 3D printed anatomically precise models of the bone structure.
They used advanced imaging software with 3D modeling and printing. Those tools helped them identify the best outcomes possible through a non-standardized surgical approach without having to make an incision. This latest endeavor represents the ever-converging synergy between orthopaedics and engineering while shedding light on the opportunities in personalized medicine.
The use of X-Ray imagery
Using specialized software, engineers can convert images from CT or MRI scans into 3D digital anatomy. Surgeons can plan their surgery using these digital models prior to making a cut, making the operation safer and more efficient. While this technology is a game-changer, the surgeon still needs to rely on their training and expertise to effectively execute the plan. This technology can also be vital in repairing previous surgeries that did not solve the patient’s problem.
The detailed digital models enable surgeons to identify various conditions by categorizing them into types and subsets, which then allows for a much more accurate surgical intervention. By using this 3D technology in advance of pediatric, adult, musculoskeletal oncology, and other cases, the surgery can be optimized to the best possible outcome.
3D printing for orthopaedic surgery

Yale surgeons, clinicians, and researchers rely on the 3D Collaborative for Medical Innovation (3DC), which is based in the Department of Orthopaedics & Rehabilitation, to create 3D printed patient-specific models and tools.
“With an in-house lab, we have many more options,” 3DC Program Director and Lead Engineer Alyssa Glennon added. “Because the 3DC is within Yale School of Medicine, we are adjacent to the physicians and the operating rooms. We can make rapid changes based on real-time feedback from the clinicians, and we can work with faster lead times since no shipment is required. We can also support more pathology types and patient age brackets, circumventing any limitations of third parties. We can have engineering staff present in the operating room at the time of surgery, or we are just a short walk away.”
Credit: Yale School of Medicine
On a very practical note, the surgeon focuses on anatomy, understanding of function, and what must be corrected, as well as a surgical approach and the hardware involved. The engineer does the processing of the CT or MRI, plus the 3D analysis, and recommends an osteotomy type and location to correct the deformity, and also virtually simulates the osteotomy and hardware placement for approval by the surgeon.
Surgery was performed in April. First the radius, which is the forearm bone that runs from the thumb side of the wrist to the elbow, was corrected and plated based on the plan, and then the ulna — the other long forearm bone — was adjusted to make sure the wrist joint was fully restored.
Remember, you can post job opportunities in the AM Industry on 3D ADEPT Media free of charge or look for a job via our job board. Make sure to follow us on our social networks and subscribe to our weekly newsletter : Facebook, Twitter, LinkedIn & Instagram ! If you want to be featured in the next issue of our digital magazine or if you hear a story that needs to be heard, make sure to send it to contact@3dadept.com