Among the wide range of 3D printing materials that can be used for medical devices, resins have often been harnessed and considered the materials of choice for dental applications. This was already considered a win for technology providers when we know that due to the expensive cost of the technology, the latter was only available to the largest, best-resourced medical centers and device manufacturers. Here is the thing, the affordability and accessibility of 3D printers came along with a demand for a variety of specifically engineered biocompatible materials with varying intended uses.
As a reminder, biocompatibility is an umbrella term for materials specifically engineered to interact with living tissues without causing an immunological response.
The challenge here lies in the ability to highlight these various intended uses, their biocompatibility certifications, post-processing technique or potential challenges that may arise during their utilization so that medical professionals can make an informed and safe decision regarding material selection. This is what this article ambitions to understand.
The majority of 3D printing resins were specifically designed for dental applications. This can be explained by the fact that when you are designing a new medical 3D printing material, there is always an application linked to this. With dental materials, there are roughly 20 applications that are quite well documented. So when you design a new material it is clear what to develop. All this information is needed when registering new material. If you develop a material for the medical sector, you can’t just design one material that is suitable for every application as it is impossible to register and get FDA or CE approval. Same as in dentistry, you would need to develop a specific material per application. But there are many more applications, that would require a high investment to develop. Additionally, all parts used for dentistry fits easily within the build volume of most resin 3D-printers, which makes resin 3D-printing perfect for digital dentistry.
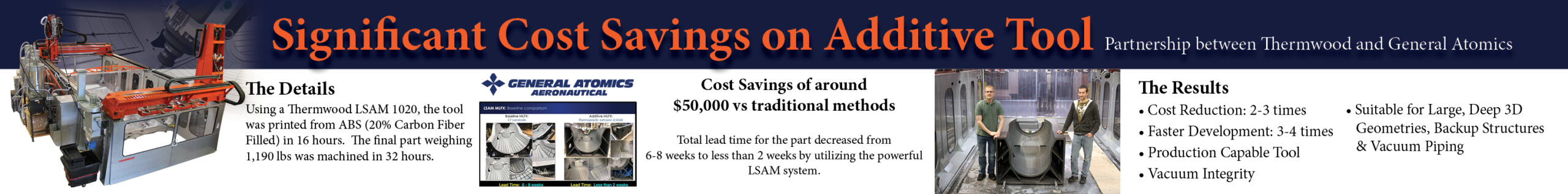
Ultimately, those dental materials – or their formulation – are being explored for other medical uses or specific medical applications. Resin 3D printing can be beneficial for applications that require patient specific customization. Among the other medical applications that are being explored right now, one notes orthopedic exoprostheses, surgical guides, hearing aids, contact lenses, intraocular lenses, specialized surgical instruments, medical models or even implants.
The question is, can resin 3D printing be used to produce end-use parts for these applications? Well, almost all of these applications may require materials for end-use parts. In some cases, like hearing aid applications, it’s possible to have end-use parts using photopolymer materials and VAT photopolymerization technology. ACS Custom for instance, a manufacturer of custom hearing protection, in-ear monitors and other communication devices quadrupled the production of custom hearing protection three years ago using resin 3D printing technologies and a specific photopolymer material.
On another note, it’s crucial to keep in mind that the selection of a material for medical applications is directly linked to the selection of the 3D printer and the requirements to meet in a given application. It turns out that depending on their final purpose, medical applications may require flexible materials, rigid materials or multiple materials.
Which type of materials for which applications?
As the majority of the materials are rigid, 3D printing turns out to be the ideal production candidate for human bones. According to research, the most common option remains acrylonitrile butadiene styrene (ABS) processed by FDM 3D printing but powders of plaster and hydroquinone were also used by Binder Jetting, as well as a mix of polyamide with glass beads by SLS. Rigid materials may also be adequate in the context of preprocedural planning, to help surgeons better prepare for the theatre room.
As far as flexible materials are concerned, one learns that the combination of SLA 3D printing with resin materials might enable the production of flexible hearts made in urethane, suitable for cutting and suturing practices without postprocessing. Whether one uses SLA 3D printing or Polyjet (with a rubber-like material mixable with a rigid photopolymer to control the flexibility of a given structure), the ultimate goal is often to create a part as realistic as possible, in order to evaluate a surgical device.
As for multiple materials, they can be combined to create a proper phantom. For some researchers, multimaterial composites should be a key area of interest in medical 3D printing applications since none of the currently available materials can mimic elastic and biological tissues.
No matter what materials are used, biocompatibility remains a primary concern for medical device manufacturers.
Assessing biocompatibility and sterilization requirements in resin 3D printing applications

If a material is intended to be used in contact with skin for 24 h for example, that material must be certified to remain chemically stable and not cause an immunological response for that duration. This seems obvious in theory.
The thing is, in practice, there are different requirements regarding biocompatibility or sterilization depending on the intended use. Biocompatibility is measured on parts with a specific manufacturing process (3D-printer, washing and post-curing). This means that biocompatible materials must be tested and certified with reference to the properties marketed by the manufacturer. When scaling-up it is important that the manufacturers’ process is exactly followed to produce biocompatible end-parts.
Nevertheless, medical professionals should be aware of the fact that sometimes, resins are broadly marketed by manufacturers as biocompatible but are supplied with either little or no detail of the specific intended uses or related certifications. Therefore, to achieve biocompatibility, they have to ensure best practice is used throughout the process by implementing a system of validation and control.
At the manufacturing level, specific process instructions from the manufacturer should be strictly followed to get the material to comply with the requirements for each application. There should be specific hardware validated, in combination with its post-processing instructions for medical resins, for example.
As another example, implantable devices are very difficult to develop and certify for that use as they are in continuous contact with the human body and blood. This is different compared to a surgical guide which is used on the short term in a wound (still in contact with blood) to make an accurate bone cut. Easier are the parts that are in contact with the skin or medical models that are only used for inspection or practice. On the side of material specifications, there are still steps to be made to mimic medical thermoplastic polymers like PEEK and PA. These thermoplastics have a long track record in medical applications. When resin with these types of properties can be printed and validated in clinical studies for long-term applications, they could open up a new era for medical 3D printing.
The reality is, for a lot of applications there aren’t any 3D-printing resins available yet. Alternatively, there might be 3D-printed metals (titanium) or SLS/FDM thermoplastics available for some applications. If an alternative ‘digital’ material is already available for such an application, the registration process is much shorter. For other applications, the resin developers and medical professionals should work closely together on each application to investigate the feasibility to digitize these processes and use resin 3D-printed parts.
This article has first been published in the March/April edition of 3D ADEPT Mag.
Authors and contributors
This article has been co-written with Liqcreate, a company that develops photopolymers for SLA and DLP technologies. Their high-end polymers are suitable for a wide range of industries including prototyping, industrial, entertainment, consumer goods, healthcare and automotive. In a previous article, 3D ADEPT Media worked with Liqcreate to shed light on the different forms of toxicity and solutions explored to reduce it in resin 3D Printing.
Other contributions include a study on “Biocompatible 3D printing resins for medical applications” and another one on “3D printing materials and their use in medical education.”