A conversation with Prof. Florian Thieringer.
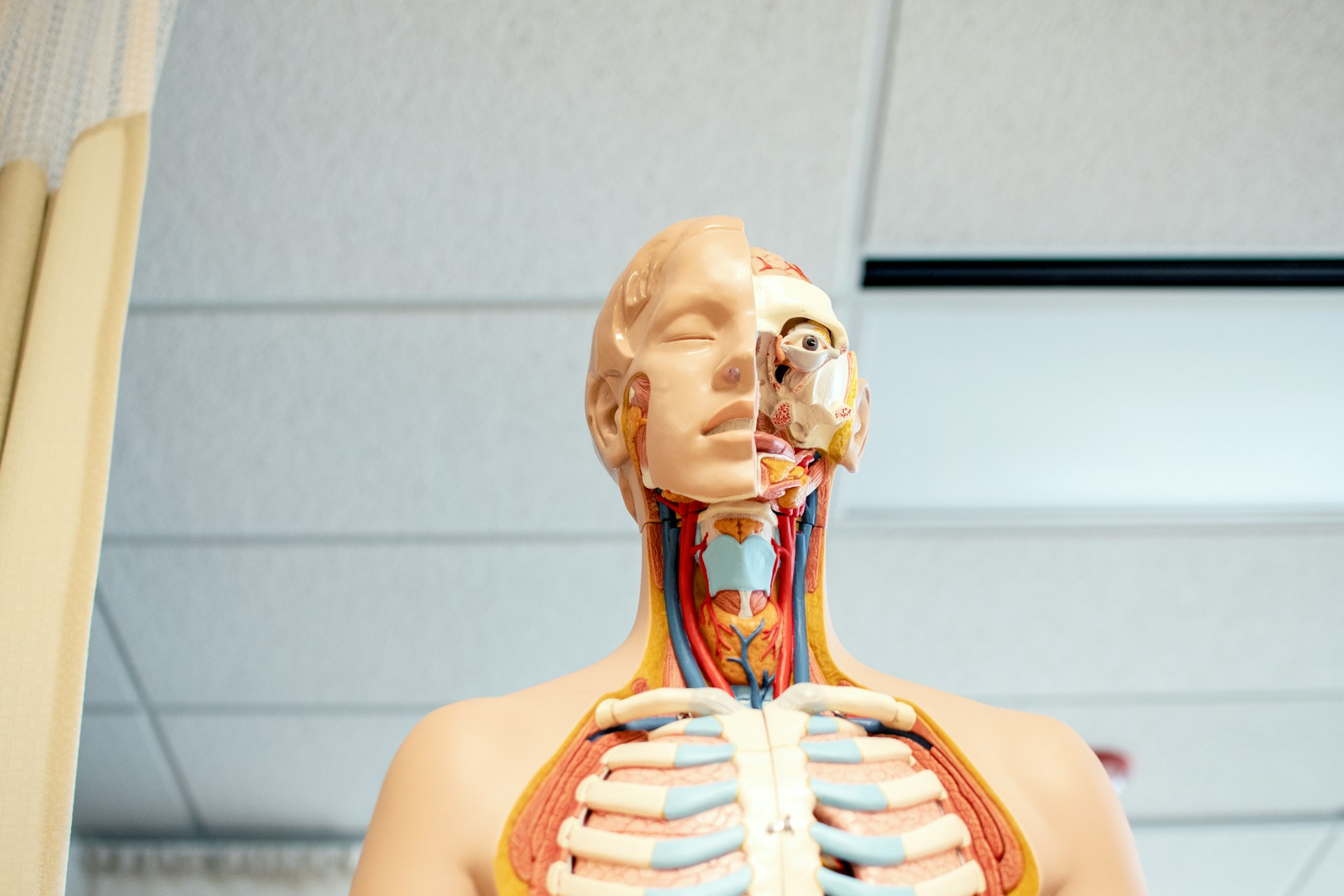
Among the wide range of specialists found in medicine, I have often called craniomaxillofacial surgeons gifted artists. Their ability to treat the soft tissue and skeletal structures of the face and skull or congenital facial malformations, as well as injuries caused by cancer, other diseases or traumatic events, is a true work of art: difficult to explain when one is not part of the field, yet beautiful and impressive. When I found out that this field of activity is the 7th out of 13 to benefit from Additive Manufacturing in reconstruction surgeries, I couldn’t help to ask myself the basic questions: What AM processes? How? Why? Given the limited number of European hospitals that rely on AM technologies for reconstruction surgeries, I reached out to Prof. Florian M. Thieringer from the University Hospital Basel, with the hope that his rich experience could help other healthcare providers take the leap on AM – or at least see this technology as a new opportunity to improve their art.
Prof. Thieringer is a man with multiple hats and outlining his various functions would probably take an entire page, so to make it simple, I would like to stick to this one: he is an Oral and Cranio-Maxillofacial surgeon and a medical 3D expert, who focuses on Tumor-, Trauma-, Reconstructive- and Orthognathic Surgery. Interestingly, the common thread across the multiple functions he holds seems to be Additive Manufacturing (AM).
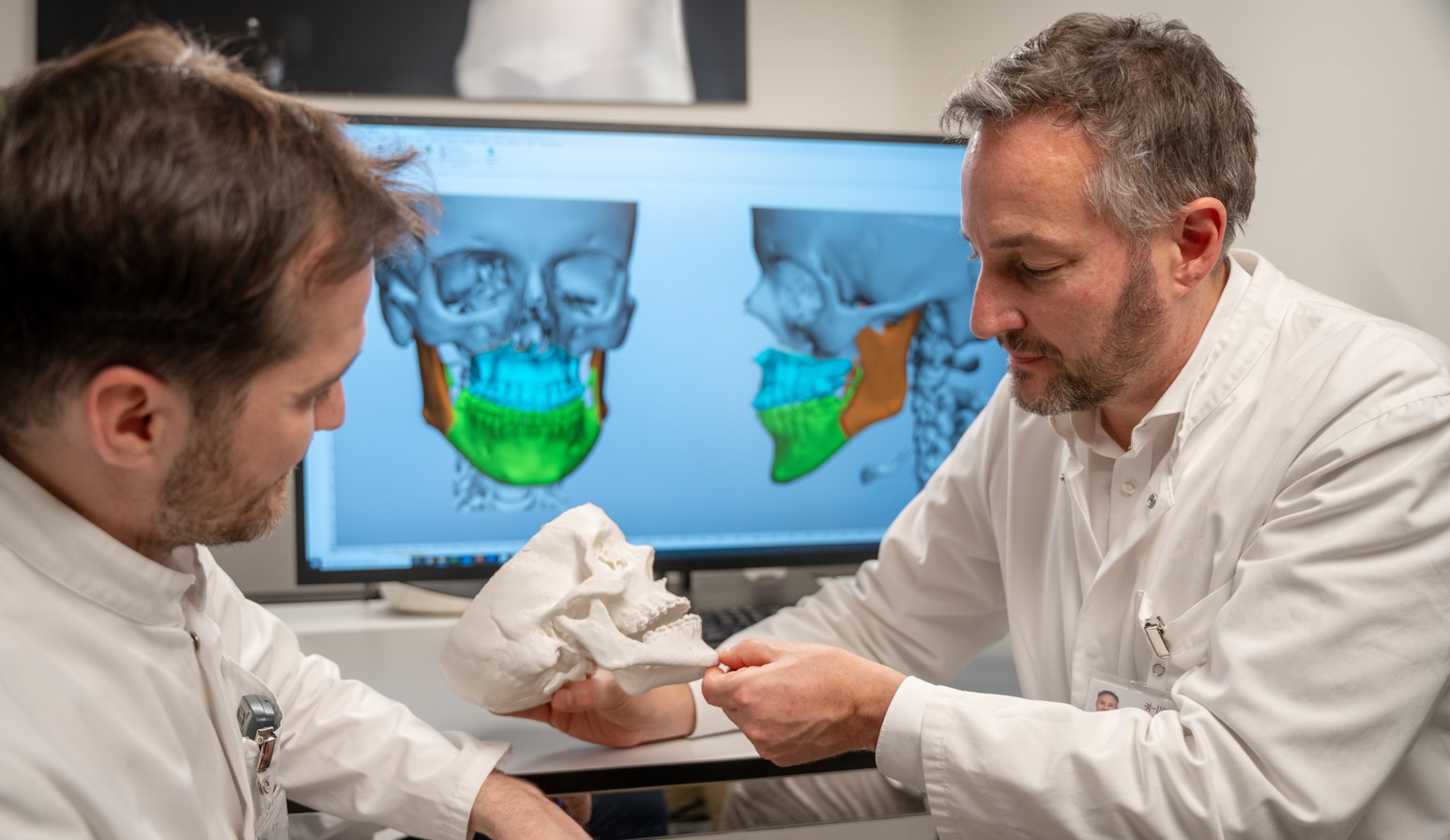
To explain the various reasons that could explain this thread, he recalls: “More than 20 years ago, when I was studying medicine, I joined the research group of my mentor Professor Hans-Florian Zeilhofer in Munich, Germany. He is one of the pioneers in medical 3D printing. Even at that time, he demonstrated that 3D printing could be very beneficial for treating our patients. With no other technology, it was possible to transfer the anatomy of a patient in a realistic, haptic, three-dimensional representation. We found it fascinating to hold the anatomy of the patients in our hands even before the operating room and very precisely plan surgical procedures.”
Even though nowadays, AM helps Pr. Thieringer and his team manufacture complex, anatomical models and patient-specific implants that fit very perfectly, it should be noted that they work with several other digital technologies along the treatment process from the very beginning until the end. “3D printing remains one of the very valuable chains of this whole process in the medical field” – alongside other digital solutions such as AR/VR or robotics.
For the sake of this article, we’ll keep the focus on its use in cranio-maxillofacial applications.

AM in reconstructive surgeries
Research reveals that AM has already been used in mandibular and orbital reconstructions, temporomandibular joint reconstruction, cranial, midfacial, cranio-maxillofacial or even auricular reconstructions.
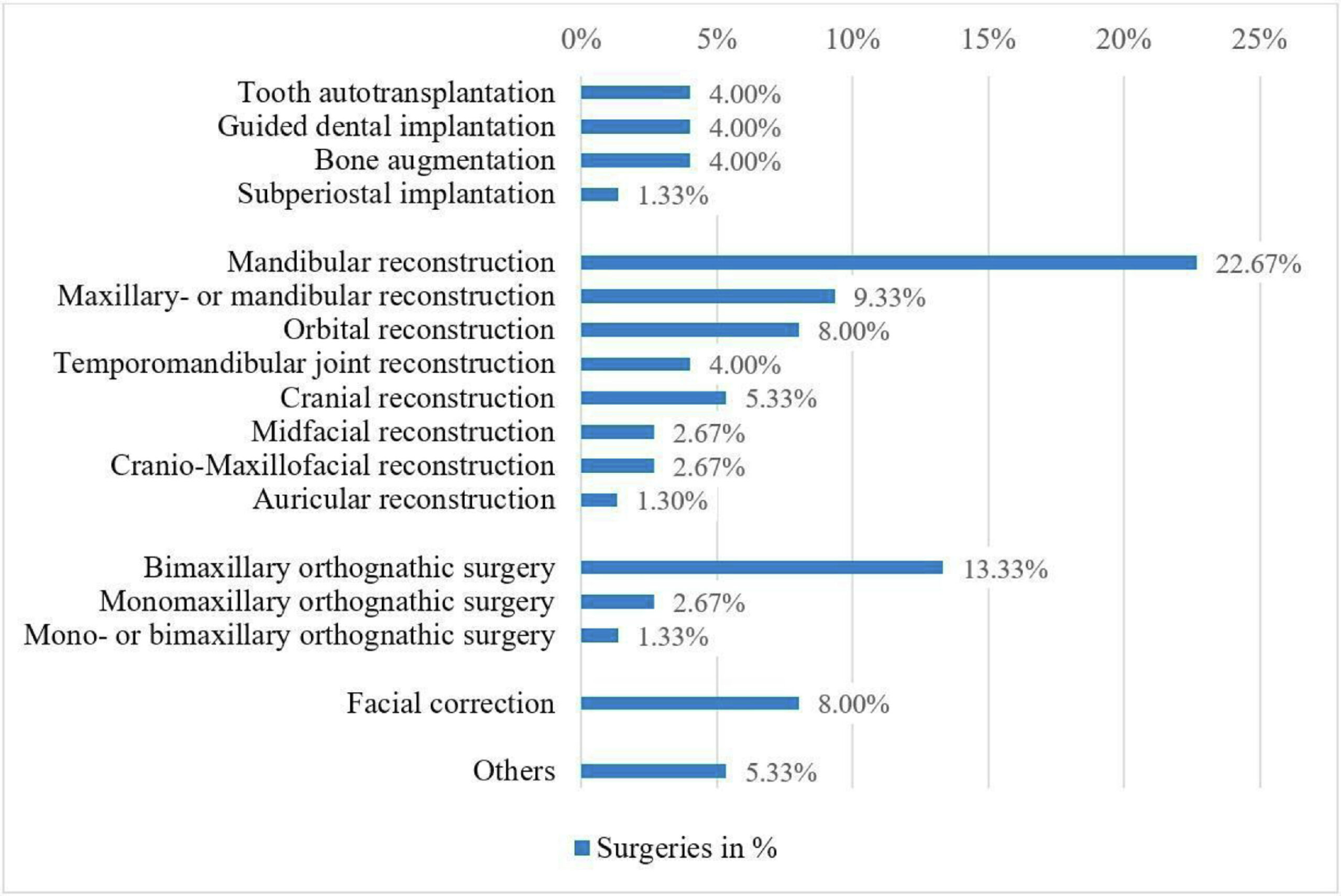
As far as cranio-maxillofacial reconstructions are concerned, high-precision models, implants, surgical guides, and fixation devices – all of which can be manufactured using AM – have proven to be valuable tools for surgeons.
“AM is a tool for challenging cases in the cranio-maxillofacial field. It’s an important part of the surgical armamentarium, therefore, the more complex the surgery will be, the more likely it is that we will use AM”, the medical 3D expert told us. Speaking of specific applications where the technology adds value, he elaborates:
“3D printing has become a standard in our clinic in the area of complex trauma. When we have patients with complex trauma injuries, we rely on 3D printing, especially when it comes to patients with orbital floor fractures and we’d like to adapt implants to our patients’ anatomy. We also use AM as a standard for our orthognathic patients who need corrective jaw surgeries.
Producing surgical guides in dental implantology or tumor surgery remains one of our key applications though. And I believe we remain one of the only international clinics that can produce patient-specific implants for direct use on the patient in the area of cranial reconstruction.”
For the expert, perfectly fitting patient-specific implants could be designed in AR/VR and be produced by intra- and extracorporal 3D printing.
[In an extracorporal 3D printing approach, the most important work occurs before the operation. The team works on a digital workflow where the implant will be designed for the patient.
In an intracorporal approach, a robotic solution will go into the head/or the place to operate and print to regenerate the defect. Pr. Thieringer explains that they can also open the skin and the printer will directly 3D print the part. While there is still ongoing bioprinting research on the topic, and given the stringent medical device regulations, the process still needs to be validated before any in-situ application.]
A possible comparison with conventional operating approaches?
So far, and in general, AM has proven to be a safe tool for craniomaxillofacial surgeons, and can sometimes deliver better results. According to the research “Medical 3D printing with a focus on Point-of-Care in Cranio- and Maxillofacial Surgery”, no study reported worse results with the aid of 3D printing. 3.14% of the studies reported comparable results to conventional approaches and 96.86% of the studies that mentioned surgical results, reported a satisfying outcome or even a better outcome with 3DP compared to conventional approaches. 93.75% of the studies that mentioned the treatment time reported shorter operations because of 3D-printed objects.
If the measuring items here are not the same as the ones used to compare AM with conventional manufacturing processes in an industrial setting, Pr. Thieringer draws attention to the fact that despite its advancement, AM remains a new approach in medicine.
“For example, to stabilize bone, an implant will be adapted during surgery. This will take a lot of time and will never be 100% accurate and perfect. So, with the so-called virtual surgical planning, and 3D printing, we benefit from the transfer of the planning time in a pre-operative setting. And with the manufacturing of perfectly fitting patient-specific implants, we can treat our patients in a totally different way.”
Needless to say, what works for one case, does not necessarily work for another.
However, from a logistic perspective, one measuring item that is found in both industrial and healthcare units is the “stock”. “By using 3D printing for every patient, you do not have to hold on to a lot of stock – in this case, traditionally manufactured implants; because each implant is produced when it is needed.”
On a more practical note, over the years, Pr. Thieringer and his team have achieved applications made from a wide range of technologies: FDM, SLA, SLM, SLS and PolyJet. As a university hospital, they probably have one of the largest fleets of 3D printers in the market.
“Every technology has its niche in the medical field. So, it highly depends on the application. We have more than 30 3D printers working for different applications. Actually, at some point, I stopped counting them. FDM for instance is being used for cost-effective anatomical models. If you just need an anatomical model in a short time or very basic models, FDM is the ideal production candidate. We also use FDM for our PEEK implants in cranial reconstruction. If you want to add additional features to your model like color or even biomechanical properties of hard- or soft tissues, or if you need transparent models, Polyjet will certainly be the ideal choice. We rely on SLM for high-performance implants made in titanium, which at the moment are still manufactured by our partners at the University of Applied Sciences. SLS is ideal for robust models or biocompatible surgical guides while SLA and DLP make sense for dental solutions”, the surgeon points out.
The adoption curve with AM

In the midst of all these healthcare fields adopting AM, digital dentistry remains the one leading the way for our guest.
The truth is the learning curve remains a tough path because of the huge need for interdisciplinary expertise. “You cannot start as a surgeon, you need engineers and technicians but not only, the traditional workflow and mindset also need to change. Adding to that the cost and regulatory aspects, one obtains a mix of items that may slow down adoption within hospitals”, the expert says.
While I am not surprised to hear these arguments, I would like to draw the attention of healthcare professionals to these cost considerations: they highly depend on several factors that are often inherent to each hospital. These factors might include personnel, budget, or even the healthcare system within their country.
What’s important to keep in mind is that you should have “a clear understanding of the clinical needs and how AM can solve them. It’s crucial as AM is not the solution to everything. Furthermore, it remains valuable to invest money in training and interdisciplinary collaboration when thinking about integrating AM in your hospital. Lastly, it’s important to navigate the regulatory side. It’s pivotal to have a risk-management system and to ensure that the processes are compliant,” Pr. Thieringer states.
In conclusion, medical 3D printing in the cranio-maxillofacial field, as showcased by Prof. Florian Thieringer’s experiences, is not just an innovative approach but a transformative force in surgical procedures. Its capacity to produce patient-specific implants and surgical guides with remarkable accuracy underscores a future where 3D printing is seamlessly integrated into clinical processes. As technology evolves and regulatory frameworks adapt, medical 3D printing will undoubtedly play an increasingly crucial role in enhancing patient outcomes and operational efficiency in healthcare. The journey of additive manufacturing from a novel concept to a standard in clinical practice is emblematic of the broader shift towards personalized medicine and digital transformation in healthcare. For Pr. Thieringer and his team “3D printing in medicine isn’t just an innovation; it’s the future of personalized patient care.”
This article has first been published in the March/April edition of 3D ADEPT Mag.